As far back as the Old Testament, midwives were heralded for their experience and knowledge. However, their story in the United States has been a constant struggle for recognition.
The full history of the American midwife is long and filled with controversy and struggle to be respected by their counterparts within the medical community. Today, the midwife is seen as an effective and empowering tool for expectant mothers. Their female-centric style of holistic care is appealing to modern women, leading to the field once again experiencing job growth.
Few occupations have seen more periods of growth and contraction throughout history. While the United States has always been a far cry from primitive societies that saw midwives as mystics that were sometimes feared to the point that they were tortured or murdered, its treatment of the midwife has been far from ideal.
The Beginning
Much like physicians, midwives in America had little in the way of regulations, standards, education or licensure to abide by until the early part of the 20th century. The debate between which is preferred – physician or midwife – goes back to the late 18th and early 19th centuries. Upper-class women in large American cities began to favor physicians, and referred to them as “male midwives.”
The interest in physicians was primarily among the rich and powerful, so it left most midwives to care for lower-class, minority and immigrant women. Over time, doctors and their new procedures became more accessible and midwives were portrayed as ignorant, dirty and illiterate.
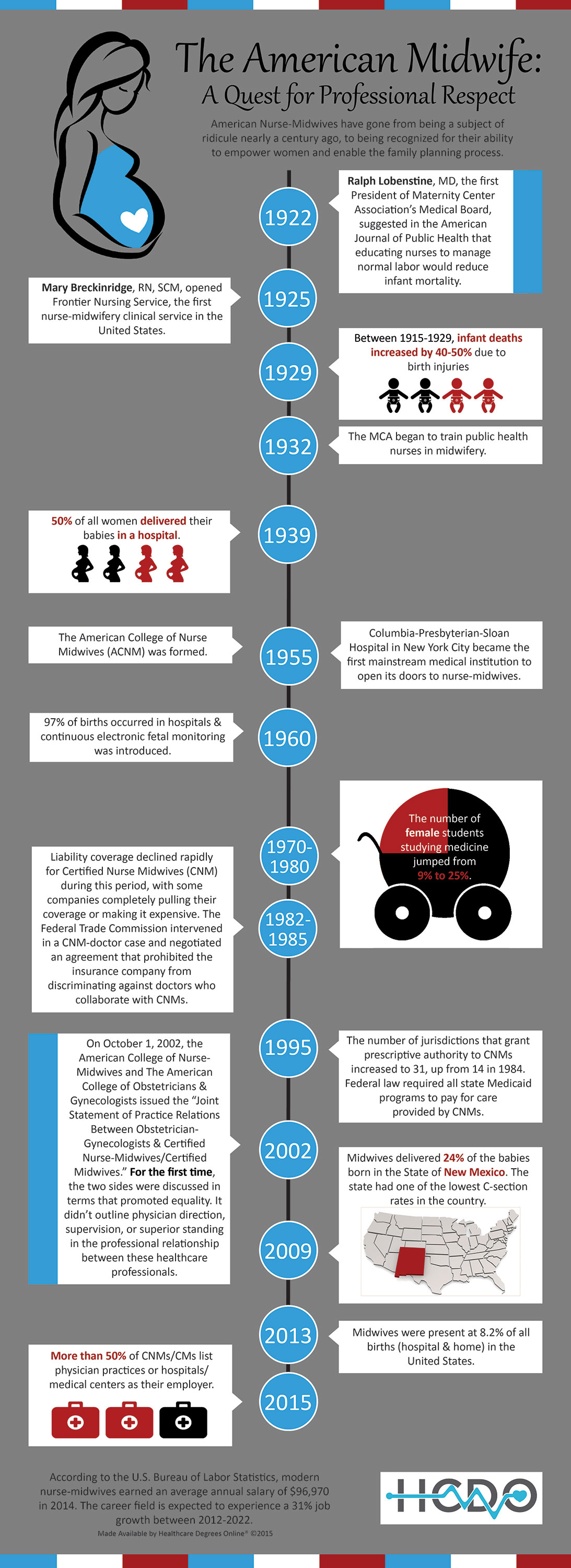
Following the 19th century, the profession was nearly abolished as childbirth became a hospitalized procedure. It took a mortality crisis for both mothers and infants in the 1920s to change perceptions of the procedures and germ-plagued facilities doctors were using. Between 1900 and 1930, pregnancy-related causes accounted for more than 15% of all deaths in women aged 15-44. The most common reason was puerperal fever, a bacterial infection of the female reproductive tract.
The mortality issue prompted a response from obstetricians, nurses and mothers, which led to the creation of a legitimate midwife profession in the American healthcare industry – the nurse-midwife.
Inspired by European counterparts, the nurse-midwife role was created to help provide women with more care during pregnancy and thus help combat the high mortality rates.
The nurse-midwife profession was largely shaped by a woman named Mary Breckinridge. A nurse herself, Breckinridge was founder of the Frontier Nursing Service, a family health services group that provided healthcare to families in rural areas around the Appalachian Mountains by sending nurses out on horseback to patient’s homes.
By 1929, Breckinridge began bringing nurse-midwives over from England. Those early professionals provided the first examples of documentable evidence that nurse-midwives reduced the rates of maternal and infant mortality and improved the health of women after pregnancy.
Legality and Practice
The creation of the nurse-midwife was not met with open arms by the obstetrics community as a whole, however. The creation of the American Board of Obstetricians and Gynecology was established in 1930, beginning an era that pitted practitioners such as midwives against specialists like obstetricians.
Midwifery was declared illegal in many places and the practice nearly died once again. For several years, it survived thanks to African-American communities in the poor, mostly rural, southern states.
These “granny-midwives” as they were called, were often the only option for African-American women who preferred to have their children at home due to the discrimination they’d face at hospitals. Granny’s would accept payments as low as two or three dollars per day to provide care. Sometimes, they weren’t paid at all. In other cases, a good day’s pay might include a chicken to take home for dinner.
Unable to eliminate the midwife practice entirely, healthcare reformers later compromised by requiring midwives to register with health departments, obtain permits and attend classes at midwife clubs and state training facilities. According to an article by Kristal Brent Zook, professor at Columbia University’s Graduate School of Journalism, this idea was still aimed at eradicating midwives altogether.
“Because of the new regulations, midwives were forced to get permission slips from licensed doctors to perform their services. Suddenly their homes had to be inspected for cleanliness, and their moral character had to be reviewed and assessed. Self-education and experience were no longer valued,” Zook wrote.
The Modern Midwife
Though healthcare reformers tried to remove them from the industry, midwives found a way to stay current. In fact, by the 1950s, nurse-midwives were becoming common at medical institutions. Colleges began standardizing nurse-midwife education and soon after, the American College of Nursing Midwives (ACNM) was created, which developed standards for practice, core competencies and certifications.
[pullquote align=”left” cite=”ACNM Philosophy” link=”http://www.midwife.org/Our-Philosophy-of-Care” color=”CC0000″ class=”” size=””]“Every childbearing family has a right to a safe, satisfying maternity experience with respect for human dignity and worth, for a variety of cultural forms, and for the parents’ right to self-determination.”[/pullquote]
In time, nurse-midwives moved toward hospital settings, ceding some of their influence over the childbirth process to the hands of doctors. Today, only 1% of births take place in the home.
The reward for doing so, however, has included the legal sanction to practice, the guarantee of appropriate physician consultation when needed and respectable wages. Modern nurse-midwives have also obtained the privilege to prescribe medications, admit patients to the hospital and receive insurance payments for their services. Nurse-midwifery is legal and regulated by licensure in all 50 states.
Over the last 35 years, interest in midwives and out-of-hospital births has risen. Their presence at births has become fairly common once again. In 2013, a midwife was present at 8.2% of births in the United States.
The Debate with Physicians Rages On
Midwives have earned higher pay as well as recognition for the quality of care they provide and the positive effect they can have in birthing outcomes. Unfortunately, there remains a sometimes combatant relationship with the physicians they now work alongside.
The primary argument is no longer about the midwives themselves, but rather home births and their safety. Midwives often accuse doctors of lacking empathy and endangering women with unnecessary procedures at the hospital. But doctors maintain that midwives allow preventable deaths of newborns and mothers in the home setting due to incompetent care.
In the end, it seems the best outcome is most often a result of the two working together. Midwives focus on the woman’s comfort and are experts in normal, low-risk pregnancies. Doctors, on the other hand, are typically more qualified to intervene in the case of a complicated pregnancy such as a C-section or pregnancies where vacuums or forceps are used to complete the delivery. As a result of their combined efforts, nurse-midwives now maintain a relationship with obstetricians, and doctors have begun to respect the effect midwives can have on the overall outcome of the entire childbirth experience.
Want to learn how to become a Certified Nurse Midwife?