 The adoption and use of electronic health records (EHRs) by hospitals and physicians has grown rapidly since the American Recovery and Reinvestment Act became law – creating Medicare and Medicaid EHR Incentive Programs – but the implementation timetables have been problematic.
The adoption and use of electronic health records (EHRs) by hospitals and physicians has grown rapidly since the American Recovery and Reinvestment Act became law – creating Medicare and Medicaid EHR Incentive Programs – but the implementation timetables have been problematic.
In response, the Centers for Medicare & Medicaid Services (CMS) recently proposed a new timeline to implement “meaningful use” for the Medicare and Medicaid EHR Incentive Programs, while the Office of the National Coordinator for Health Information Technology (ONC) proposed a more regular schedule for updating its certification regulations.
With the proposed timeline changes, Stage 2 will continue through 2016 and Stage 3 will follow, beginning in 2017 for healthcare providers who have spent two years in Stage 2.
The intention behind the proposed change is to allow Stage 2 to be implemented successfully and to use the data collected during this stage to make decisions for Stage 3.
Here’s what the CMS had to say:
“The phased approach to program participation helps providers move from creating information in Stage 1, to exchanging health information in Stage 2, to focusing on improved outcomes in Stage 3. This approach has allowed us to support an aggressive yet smart transition for providers.”
The CMS said the changed timeline will be beneficial in allowing for additional stakeholder feedback for the ongoing progress and eventual outcomes of Stage 2; increased data collection during Stage 2 and time to adjust calculations; more time to consider Stage 3 options; added time for enhancement and preparation of Stage 3; and the time developers need to create EHR technology and get it distributed.
Meanwhile, the ONC proposed a new regulatory approach to allow for more frequent certification criteria updates. Those changes are designed to allow for public input on policy proposals, enable certification processes to better adapt to changing industry stands and give EHR developers more predictability.
So why are EHRs important?
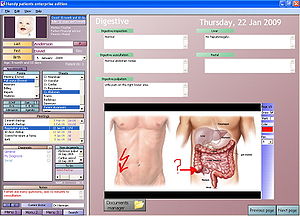
EHRs — basically a digital version of a paper chart containing all of a patient’s medical history — will affect every patient in the United Station, wrote Tom O’Hanlan, a board member of Baptist Easley Hospital in the Greenville (S.C.) News. The EHR gives patients, physicians and other healthcare providers access to a patient’s medical records across facilities, helps providers diagnose and treat patients by tracking data, identifies patients due for preventive visits and screenings and monitors how patients meet certain parameters.
In other words, an EHR can improve a practice’s overall quality of care, O’Hanlan wrote.
The changes met with a mixed review.
While most industry organizations supported the extra time, not everyone is pleased with the changes.
“We have been against delaying implementation the subsequent stages each and every time, and we are against this delay,” Dan Haley, VP of government relations at athenahealth, told govhealthit.com. “The fact that the delay is necessary is really a public policy failing.”
Some wanted additional flexibility with Stage 2.
“There is a perfect storm brewing,” said College of Healthcare Information Management Executives (CHIME) CEO Russ Branzell in a statement. “With ICD-10 compliance coming into view, with HIPAA compliance demanding renewed attention and with all the activities associated with the Affordable Care Act converging in 2014, providers are nearing a breaking point. Flexibility of the kind announced today is beneficial for Stage 3, but Stage 2 start-date flexibility is needed to ensure long-term success.”